Baby and Newborn Colic Relief
Baby and Newborn colic is a functional gastro-intestinal disorder (FGID) with elusive pathophysiology and multifactorial in nature3. Defined as ‘an infant <5 months of age with recurrent and prolonged episodes of crying, fussing, or irritability that occur without obvious cause and cannot be prevented or resolved by caregivers’3.

Health implications
Initially thought to be transient in nature, infant colic has now been linked with increased risk of developing other functional gastro-intestinal disorders like IBS1, atophy-allergy4, asthma5 and behavioural problems6 later in life.
Limitations
Colic remains a diagnosis of exclusion, perhaps a reason why conventional approaches have failed7. Treatments for reflux like proton pump inhibitors (PPIs) have not been found effective at reducing crying8. Simeticone (Infacol) has been found no better than placebo9. Current guidelines consist of coping strategies for parents1,7.

Craniosacral therapy for Baby and Newborn Colic Relief
Craniosacral therapy (CST) has increasingly been adopted by parents as a safe and effective method to help solve colicky symptoms10.
Following a session, parents find ‘a more relaxed baby, that cries less, digests better, is more contented and restful and needing less comfort’.
The added benefit is less parental anxiety, better bonding and an overall improved parental experience. This may partly due to the therapeutic effect of the practitioner in reassuring and supporting parents during challenging times7.

The Science
There is positive evidence that CST is effective at reducing crying and increasing sleep.
A trial of 28 infants found after 4 treatments a statistically significant reduction in crying (P<0.001), and sleep (P<0.002) versus no treatment. Overall differences between the treatment and control group was a decline in crying of 63% and 23% and improvement in sleep of 11% and 2% respectively11.
A trial of 43 infants compared CST to another manual therapy over 4 weekly treatments. At day 14, the mean change in hours of crying by day in the CST group was by 2.5 to 1.5 h/day, (p < 0.001) and increase in hours of sleep by 1.0 to 1.8 h/day, (p< 0.01)12.
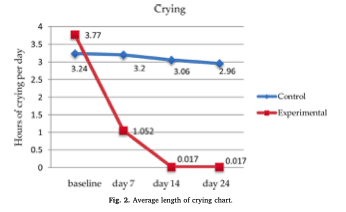
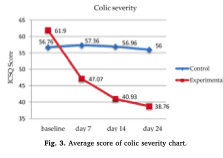
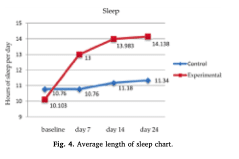
Results from a larger RCT in 2019 further support the clinical effectiveness of CST. 58 colicky infants aged 10-90 days were randomised to the intervention (4 CST treatments over 24 days) and control group (parental advice solely). Graphs below show a significant reduction crying duration, colic severity and sleep13
How does Craniosacral therapy work for baby and Newborn colic Relief
According to craniosacral principles, colicky symptoms and excessive crying of the infant can be the result of unresolved compression of the base of the skull due to birth dynamics, causing dysfunction of cranial nerves and affecting various organs including the gastrointestinal tract.
It can also impact higher functions e.g. sleep, alertness and ability to soothe/process emotions14.
The trained therapist’s palpation skills and light touch gets rid of tension and restriction in the head, neck, diaphragm, joints and tissues allowing for the restoration of normal nerve function.
Conclusion
Is craniosacral therapy effective at reducing colic? There is increasing evidence of craniosacral therapy in terms of crying reduction and increased sleep.
In general, manual therapy (i.e. craniosacral therapy and others) is increasingly popular and it is being integrated in the healthcare sector due to positive reports from parents and clinicians as well as its safety record.
Do you want to know if your baby is colicky? Take this 2-min free Baby Colic questionnaire to find out and determine the next steps to resolve your baby’s fussiness.
References
1. Zeevenhooven et al., 2018. Infant colic: mechanisms and management. Nat Rev Gastroenterol Hepatol 15, 479–496. http://doi.org/10.1038/s41575-018-0008-7
2. Vandenplas et al., 2015. Prevalence and Health Outcomes of Functional Gastrointestinal Symptoms in Infants From Birth to 12 Months of Age. J Pediatr Gastroenterol Nutr. 2015 Nov;61(5):531-7. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4631121/
3. Zeevenhooven et al., 2017. The new Rome IV criteria for functional gastrointestinal disorders in infants and toddlers. Pediatric 1. Gastroenterology, Hepatology and Nutrition, 20(1), pp. 1-13. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5385301/
4. Danielewicz et al., 2017. Diet in pregnancy—more than food. European Journal of Pediatrics, 176(12), pp. 1573-1579. http://www.researchgate.net/publication/320838698_Diet_in_pregnancy-more_than_food
5. Thorburn et al., 2015. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nature Communications, Volumen 6. http://www.nature.com/articles/ncomms8320
6. Loughman et al., 2020. Infant microbiota in colic: Predictive associations with problem crying and subsequent child behavior. Journal of Developmental Origins ofHealth and Disease. http://www.thelancet.com/pdfs/journals/ebiom/PIIS2352-3964(20)30015-3.pdf
7. Ellwood et al., 2020. Comparison of common interventions for the treatment of infantile colic: A systematic review of reviews and guidelines. BMJ Open, 10(2), pp. 1-13. http://bmjopen.bmj.com/content/bmjopen/10/2/e035405.full.pdf
8. Mai, T. et al., 2018. Infantile Colic: New insigth to an old problem. Gastroenterology Clinics of North America, 12, 47(4), pp. 829-844. http://pubmed.ncbi.nlm.nih.gov/30337035/
9. Biagioli et al., 2016. Pain-relieving agents for infantile colic. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No.: CD009999. http://www.cochrane.org/CD009999/BEHAV_pain-relieving-agents-infantile-colic
10. Carnes et al., 2018. Manual therapy for unsettled, distressed and excessively crying infants: a systematic review and meta-analyses
BMJ Open 2018;8:e019040. http://bmjopen.bmj.com/content/8/1/e019040.citation-tools
11. Hayden et al., 2006. A preliminary assessment of the impact of cranial osteopathy for the relief of infant colic. Complementary therapies in clinical practice. 12. 83-90. 10.1016/j.ctcp.2005.12.005. http://www.researchgate.net/publication/7133428_A_preliminary_assessment_of_the_impact_of_cranial_osteopathy_for_the_relief_of_infant_colic/citation/download
12. Browing et al., 2008. Comparison of the short-term effects of chiropractic spinal manipulation and occipito-sacral decompression in the treatment of infant colic: A single-blinded, randomised, comparison trial. Clinical Chiropractic. http://doi.org/10.1016/j.clch.2008.10.003
13. Castejón-Castejón et al 2019. Effectiveness of craniosacral therapy in the treatment of infantile colic. A randomized controlled trial. Complement Ther Med. 2019 Dec;47. http://pubmed.ncbi.nlm.nih.gov/31780018/
14. Kotzampaltiris et al., 2009. The cranial rhythmic impulse and excessive crying of infancy. J Altern Complement Med. 2009 Apr;15(4):341-5. http://pubmed.ncbi.nlm.nih.gov/19368513/
Photos 1 & 3 by Kelly Sikkema on Unplash
Photo 2 by Tim Bish on Unplash
Photo 4 My 3rd child 🙂