Is your baby fussy or crying? hard to settle? You want to know if it is colic or something else…But most of all, you want immediate relief for your baby.
The journey has not been easy. You have come across different opinions. In addition, you have already tried different methods to relieve colic without success and at this point, you are probably confused and maybe shattered.
Here is my message: you are not failing and it is not your fault! In the past 8 years, I have worked with many parents struggling through broken sleep, exhaustion and helplessness in the face of colic. The truth is that the root causes of colic are many and so are the choice of cures.
I have put together the guide Baby Colic: root causes, natural cures backed by the latest science and my clinical experience. Understanding the root causes of colic s is the first step towards understanding your baby’s behaviour. This in turn, will help you make informed choices about the best approach to bring relief to your baby.
Table of contents
What is colic
1. Definition
Infant colic is defined as ‘recurrent and prolonged episodes of crying, fussing, or irritability in an infant that is less than 5 months old that occur without obvious cause and cannot be prevented or resolved by caregivers’ (1).
Colic occurs in healthy babies. Hence, it is not a medical condition (not a disease) but rather a syndrome (a constellation of symptoms without known cause, course or treatment). Just like IBS (irritable bowel syndrome), the idea of colic as a baby IBS is gaining weight (2).
In truth, the direct cause of colic is not known. Hence, the diagnosis is purely based on signs and symptoms (3). The tricky thing is that signs and symptoms in a young baby are difficult to quantify and every baby’s colicky symptoms seems to be unique in his/her own way. Needless to say, this leads to confusion among parents and medical/health practitioners, e.g.
- Is it colic?
- Is it reflux?
- Is my baby in pain?
- Is it milk allergy?
- Is there a problem with my milk?
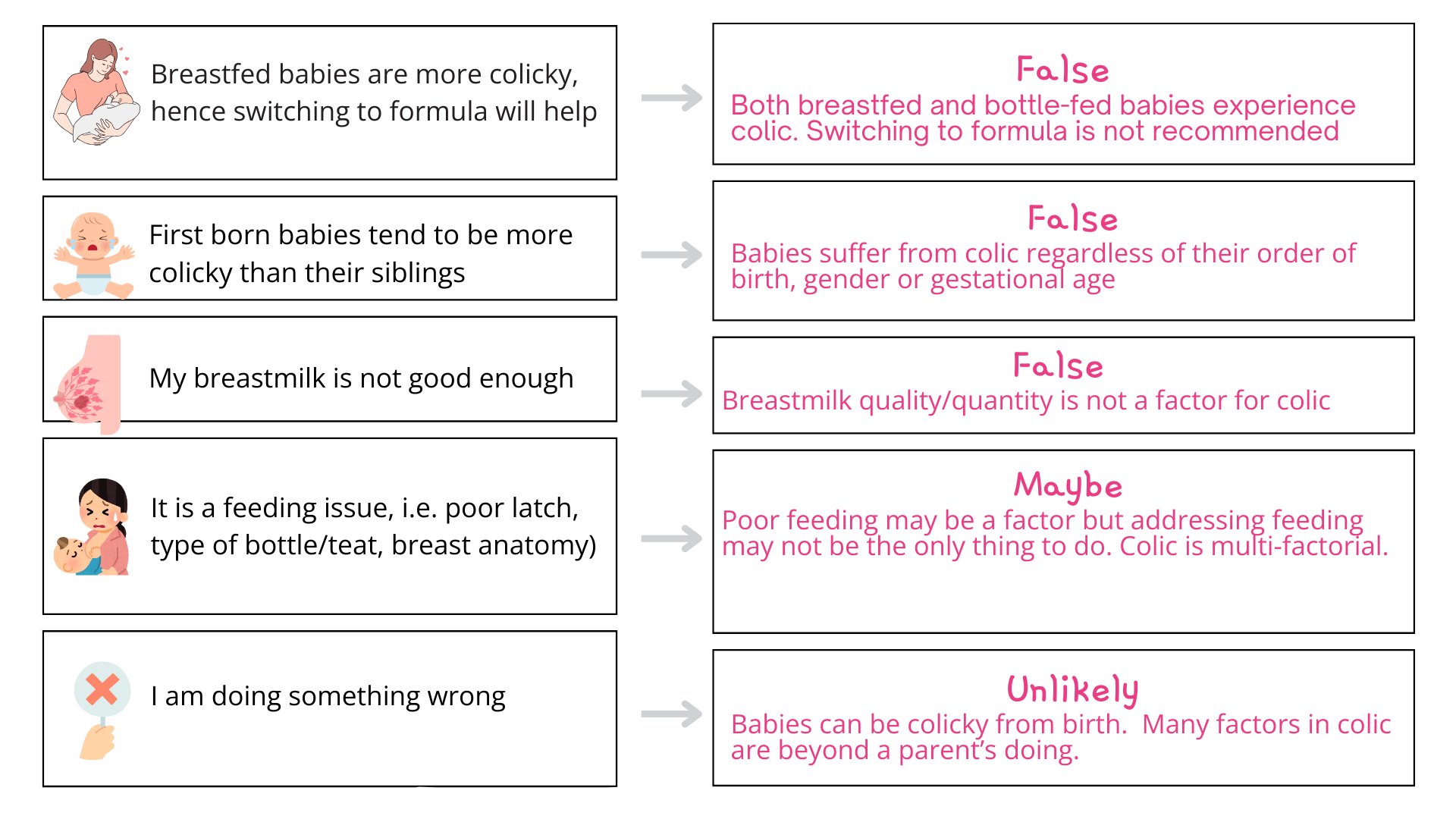
2. Myths
Over the years, this general confusion has generated a number of myths.
Relevance
Actually, infant colic has a larger impact than initially thought. It is currently estimated to:
- affect up to 25% of newborns under 3 months of age (4)
- be the main cause of GP visits during the first year of life (5)
- be a major reason for stopping breastfeeding (6)
- affect bonding and attachment as it diminishes a parent’s sense of self-efficacy and competency to care for a baby (7)
- lead to considerable psychological, emotional and physical suffering for parents and babies (8)
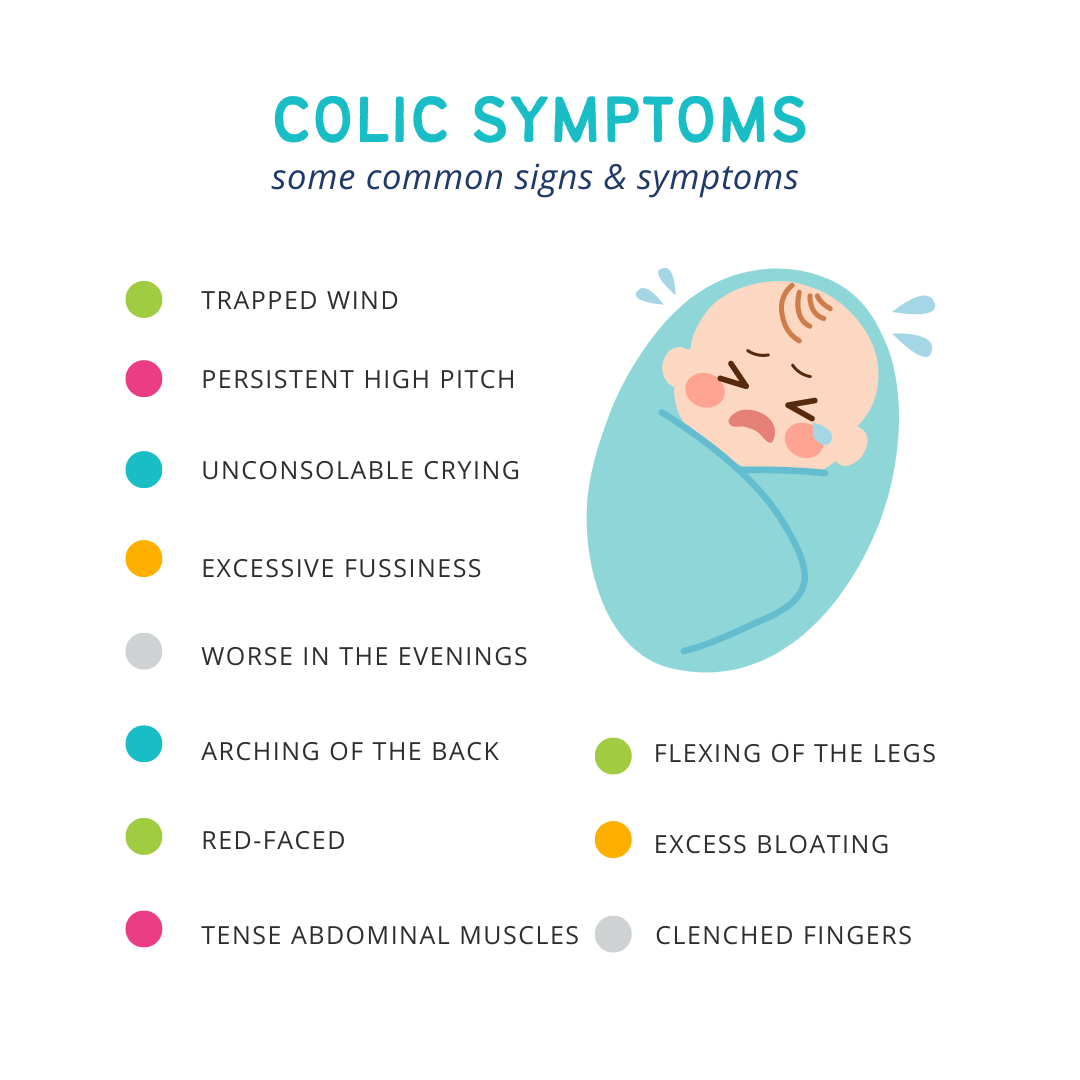
Signs and symptoms
These are the most common signs and symptoms of colic as reported by parents and clinicians (9).
Symptoms requiring immediate medical attention are (10):
- Severe distress
- Appears sick or lethargic
- Failure to thrive
- Green vomit/stools
Limitations of current approaches
Limitations of current approaches are due to the fact that NEW science into root causes and natural cures of colic is generally NOT part of clinical practice.
This gap between science and practice contributes to:
1. Poor understanding of the onset of colic
It is still believed that colic starts at around 3 weeks, peaks at 6-8 weeks and declines progressively until about week 12 (11). However, recent evidence shows that it can actually start from birth (12). This is significant as some early colicky behaviours of newborns may have been misinterpreted (i.e. baby cries as baby is hungry) or dismissed (i.e. a fussy, clingy baby).
2. Poor understanding of the symptoms
Many clinicians and public guidelines use the ‘rule of 3’ to diagnose colic (13). That is, a baby has colic if baby cries or fusses more than 3 hours a day over 3 days in a week. However, the current view is that colic can not only be defined by the number of hours a baby cries (14). To continue using the old-fashioned ‘rule of 3’ (which was firstly described over 70 years ago!) (15) may miss a large number of colicky babies with milder symptoms.
3. Poor understanding of the long-term health impacts of colic
Medical practitioners presently advise parents that colic doesn’t require medical attention as the baby will ‘grow out of it’ (16). However, there is evidence that colicky babies have increased risk of developing atophy-allergy (17), asthma (18) and behavioural problems later in life (19). In addition, a recent study of colicky babies (nearly 360,000) versus non-colicky (363,000) showed that those with colic had a higher risk of developing IBS at 4 years of age (20). These risks are too compelling to be dismissed.
4. Poor effectiveness of treatments for colic
Doctors typically try a number of approaches in an attempt to help the distressed baby (21). These may or not work. As a result, the journey of a parent of a colicky baby is often (as reported by parents) filled with confusion and distress in the search for quick relief. Indeed, experts have alerted that ineffective approaches lead to more medical visits which then result in doctors over-prescribing medications to young babies and anxious parents exploring all kinds of commercial solutions (22).
5. Diagnostic confusion
The way a baby is defined as colicky is highly subjective. For a starter, the definition of colic is vague, it relies on the experience of the doctor/clinician as well as reports from the parents. This situation oftentimes leads to diagnostic confusion. In practice, colicky babies tend to be categorised in one of these 3 areas which have overlapping symptoms that are generally attributed to colic (see diagram below):
- Cow’s milk protein allergy (CMPA)
- Reflux/regurgitation
- Issues with lactose
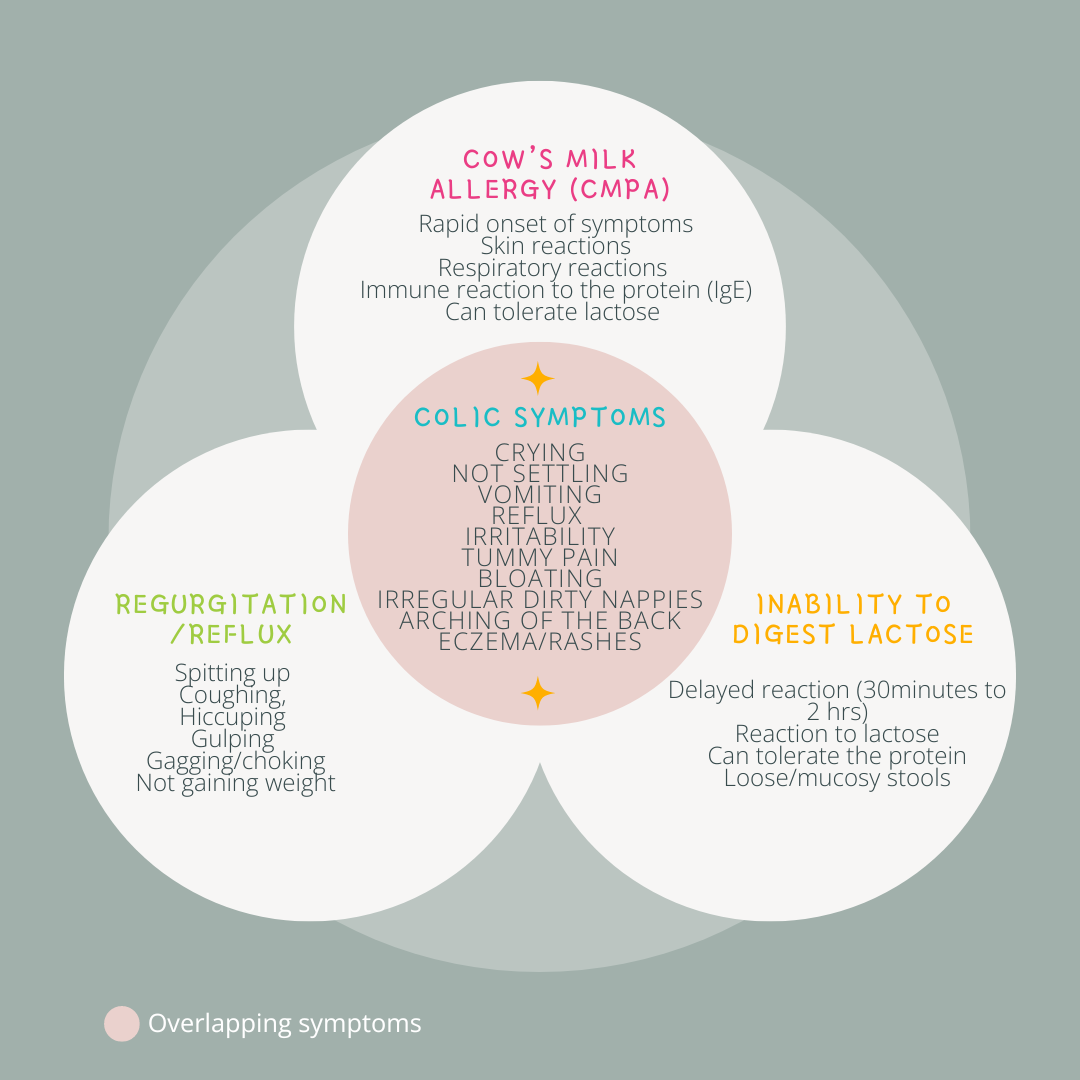
Cow’s milk protein allergy (CMPA)
It is common to think that fussy babies cannot digest milk and hence there is probably an allergy. Cow’s milk protein allergy (CMPA) is a medical condition. It is true that CMPA can mimic colic symptoms. However, if a baby CMPA is confirmed then colic is ruled out. CMPA can be tested by doctors via a skin prick test that looks for an IgE-type (immune) of reaction. Oftentimes, CMPA is diagnosed just by signs and symptoms. This practice has been found to lead to over-diagnosis (23).
Inability to digest lactose
The inability to digest lactose, a naturally occurring sugar found in breastmilk and formula is common in babies yet it is not generally considered a cause of colic. Lactose is digested in the baby’s gut by an enzyme called lactase. Some babies are born with the inability to produce this enzyme (rare). Most commonly, some babies are born with a lower capacity to produce this enzyme. As the baby’s gut matures, their ability to produce lactase may improve. Concurrently, the growth certain species of bifidobacteria and lactobaccilus in the baby’s gut may help to digest lactose (24). When lactose is not fully digested, gut bacteria can ferment on it producing gas (hydrogen, carbon dioxide, and methane). This can result in tummy discomfort (the level of discomfort depending very much on individual levels of tolerability).
Regurgitation/reflux
Regurgitation such as spitting up during or after a feed is part of the normal development of a baby and is generally considered harmless (25). Refluxy/colicky symptoms can manifest simultaneously and share common traits. In addition, regurgitation is often mistaken for reflux (26). Many fussy babies may be diagnosed with reflux and given reflux suppressant medications.
New approaches
Fortunately, scientists are advancing the causes of colic. In essence, it is about the correct maturation of the gut and brain (the baby’s nervous system). There are a number of factors that can affect the optimum development of the gut and brain in a baby and hence, contribute to colic onset.
Contributing factors can be grouped in 3 main blocks as shown below.
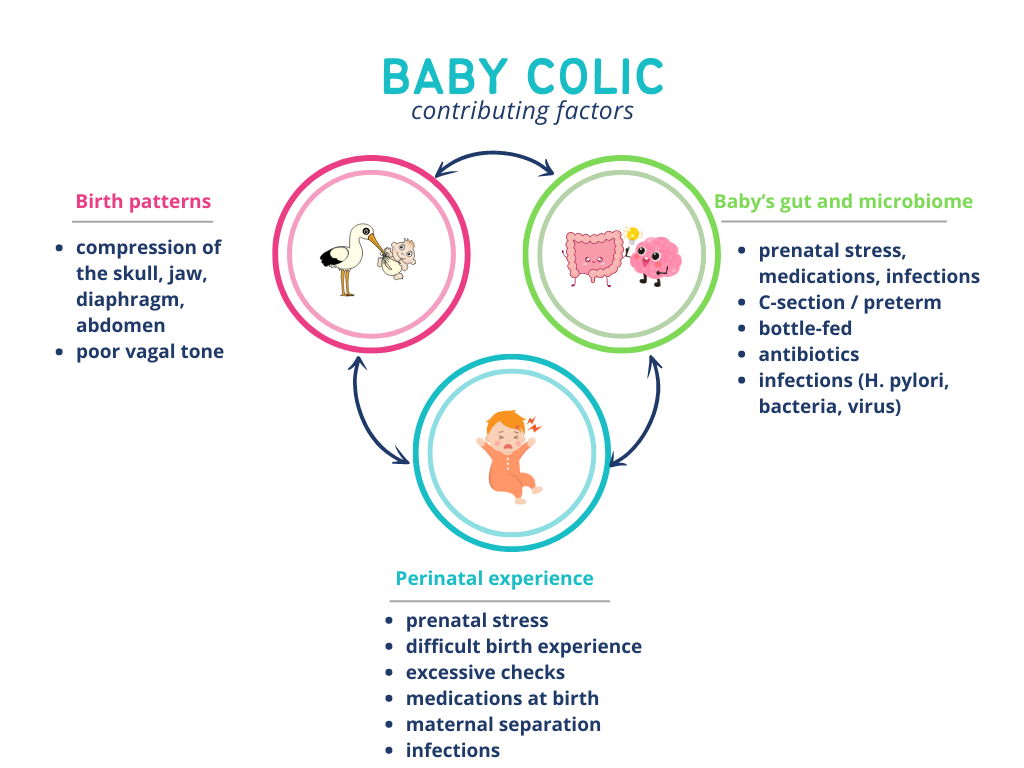
1. Birth patterns
Birth forces can cause compression in babies head, abdomen and pelvis. In babies, the vagus nerve is of key importance. The vagus runs on both sides of the neck, meets at the level of the chest bone and connects every single organ of digestion. The compression forces of birth can put a strain on this nerve and affect feeding, digestion and general contentment.
Some examples of unresolved compression due to birth leading to symptoms in babies:
- on the base of the skull and jaw, it can affect sucking, swallowing, burping, latching (27)
- On the diaphragm, it can drive reflux/regurgitation by pushing the stomach through the diaphragm or leave a diaphragm that is too tight.
- On the abdomen, poor vagal tone can contribute to poor digestion, bloating, excess gas, constipation, colic, pain
- it can also impact sleep, alertness, mood and the ability to soothe/process emotions (28).
2. Baby’s gut and microbiome
When babies are born, they do not have a stable microbiome (the combination of healthy organisms in their gut) (29). The first year of life is essential for the successful colonisation and maturation of these healthy bacteria. Colicky babies have a different composition of gut bacteria than non-colicky babies (30). In particular, they present with types of bacteria that can cause inflammation (cramping, pain) and excess gas (bloating, fussiness) (31).
What prevents the favourable growth the baby’s microbiome? (32):
- C-section / preterm
- bottle-fed
- antibiotics
- infections (H. pylori, bacteria, viruses)
3. Perinatal experience
How babies are received into the world and their experiences in the early days can influence a baby’s sense of safety and impact behaviour (33). Adverse experiences such as maternal stress during pregnancy and some perinatal events like excessive checks, medications, maternal separation or infections can leave the baby’s nervous system feeling unsafe (34). This can suppress the vagus nerve and lead to symptoms that qualify a baby as ‘fussy’, ‘unsettled’ or ‘colicky’.
Some examples of ‘low vagal tone’ in a baby:
- Tummy discomfort or pain
- Frequent waking or unable to relax/take naps
- restlessness
- irritability
- over-alertness
- over-responsive to their environment (loud noise, bright lights)
- poor sleep
- difficulty breastfeeding/refusing the breast
- clinginess
- upsets easily
- hard to calm down. excessive crying can also be a way to express strong emotions
Natural cures
Since the causes of colic are many, so are the cures. There is a difference between soothing approaches, which can provide temporary relief and root cause approaches which have the ability to redress the contributing factors and set things right for the correct development of the baby’s gut and brain.
1. Root cause approaches
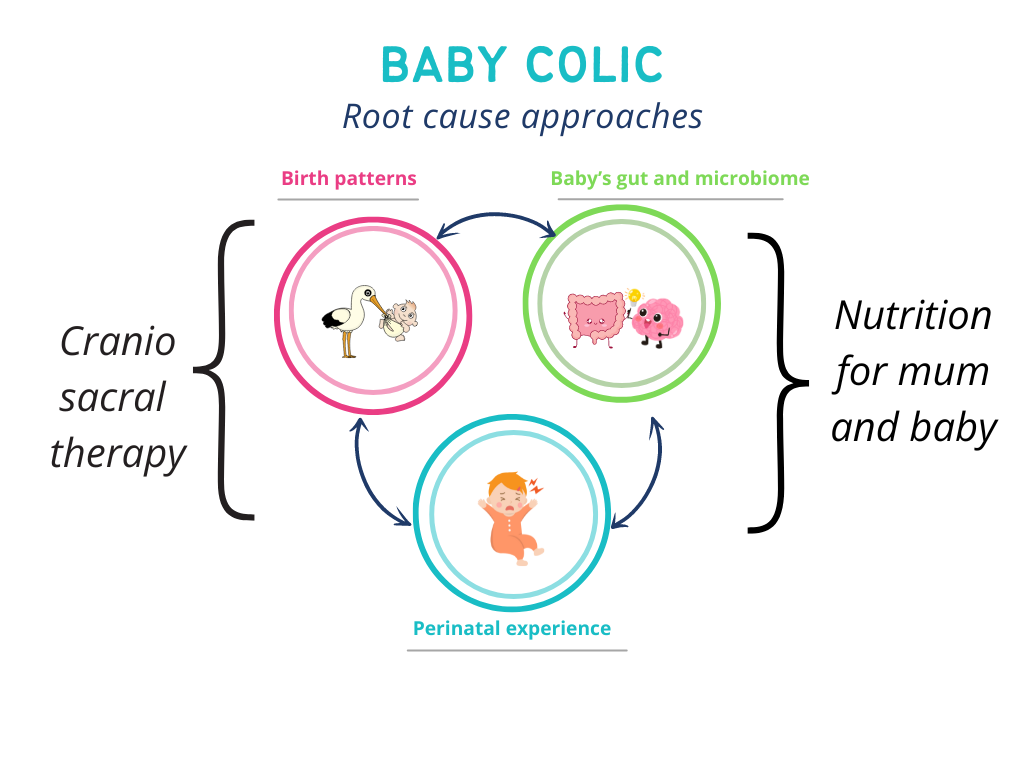
Craniosacral therapy (CST)
CST can address several contributing factors of colic. The CST therapist’s palpation skills and light touch can rid of tension and restriction in the baby’s head, neck, diaphragm, joints and tissues allowing for the restoration of normal vagus nerve and organ functions. In addition, a CST therapist offers empathic listening and presence, which can help release the stress associated with strong experiences.
It has increasingly been adopted by parents as a safe and effective method to help solve colicky symptoms(35). Following a session, parents find ‘a more relaxed baby, that cries less, digests better, is more contented and restful and needing less comfort’ (36).
Moreover, there is evidence that CST is effective at reducing crying and increasing sleep. A recent randomised controlled trial demonstrated that 3 CST sessions over 2 weeks were sufficient to significantly reduce crying hours and resolve colic in 58 colicky babies (37).
In conclusion, the combination of positive evidence and feedback from parents as well as its safety record (38) makes CST a valuable therapy to resolve colic.
Nutritional support to the breastfeeding woman
In breastfed babies, it is a common belief that some foods women eat can have a negative impact on their babies, namely dairy and cruciferous vegetables (39). Nevertheless, these popular beliefs have been backed by science. A reduction of crying hours, gas production and inflammation were found following the elimination in the maternal diet of:
- cruciferous vegetables (40)
- wheat, soy and dairy (41) (42)
- FODMAPs FODMAPs (fermentable oligo, disaccharides, monosaccharides and polyols) (43)
Moreover, what mums eat has the potential to shape the health of their babies. Recent studies show how breastmilk composition can be affected by diet (44). As regards colic, it has been observed that breastmilk richer in healthy fats (omega 3 long-chain poly-unsaturated fatty acids-PUFA) are associated with reduced distress in babies (45). There are indications that these healthy fats promote the growth of beneficial bacteria, have an anti-inflammatory effect in the baby’s gut and serve to develop a healthy brain (46).
In conclusion, breastfed babies with colic symptoms may benefit from the removal of certain foods from their mother’s diet. At the same time, maternal diets need to be balanced for optimal breastmilk quality. Given the difficulties parents face at this highly demanding time, it is sensible that they seek advice from a nutrition expert.
Nutritional support to the colicky baby
It is well known that probiotics can provide colic relief and at the same time introduce long-lasting positive effects in the maturing baby’s gut (47). In concrete, certain species of bifidobacterial and lactobacilli may have the potential to reduce inflammation, prevent the growth of unwanted bacteria, promote tolerance to cow’s milk, digest lactose and regulate bowels in both breastfed and bottle-fed colicky babies (48).
A word of caution, the efficacy of baby probiotics for colic relief depends on selecting the right type bacteria for the right problem. For example, the extensively studied L. reuteri (that goes with the brand name Biogaia) seems to be mostly effective in exclusively breastfed infants (49). Recent discoveries show that the combination of probiotics (live bacteria) and prebiotics (beneficial fibres) may be most effective (50).
In conclusion, probiotics and prebiotics have the potential to provide relief to the colicky baby. They have a good safety record too. Many commercial options are available. It may be advisable to get advice from a nutrition expert to choose the best combination of bacteria.
2. Soothing approaches
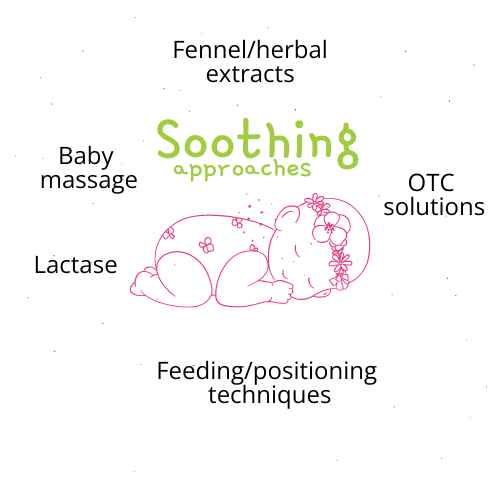
Fennel and herbal solutions
Herbal extracts and colic teas have long been used for digestive problems for young and old. Parents of colicky babies report quick relief with no adverse effects (51). Herbal products typically involve herbs such as chamomille, fennel, anise or melissa. In concrete, fennel (seed oil extract and tea) has shown to provide significant relief, i.e. less crying, less discomfort and less colicky episodes in several trials (52). Fennel is an antispasmodic, which means that it helps to relax the gut muscles and thus helps with cramping and trapped wind (53). Additionally, fennel is galactalogue (a natural compound that stimulates milk production (54), which is why it is recommended during breastfeeding.
In conclusion, herbal extracts including fennel can help a colicky baby and are generally safe. The exact proportion and/or combination of herbal extracts for colic relief remains uncertain (55). Hence, it can be a hit and miss.
Feeding and positioning techniques
Feeding, positioning, including burping and winding techniques can help ease the symptoms of poor digestion and help baby feel more satisfied after a feed. They constitute simple coping strategies for parents close to rocking, bathing, the use of soft music and/or white noise. However, they do not tackle the root cause of colic (56). Improving feeding in breastfed babies can definitively support mum to breastfeed for longer. However, there is no evidence that poor latch or incorrect positioning leads to colic. As a matter of fact, both breastfed and bottle-fed babies develop colic in similar numbers.
In conclusion, feeding, positioning strategies may help momentarily. Other approaches may be needed to help resolve colic from its roots.
Baby massage
Baby massage benefits both parent and baby in terms of bonding and relaxation (due to oxytoxin release) which can indirectly help with feeding and sleep. Parents who practiced regular massage to their newborns were found to be less anxious (57).
Massage can have a positive gut-brain effect. It provides safety cues and reassurance for the baby’s nervous system, i.e. eye to eye contact, smiles, nurturing touch, cuddling, soothing sounds and pleasant smells. On the gut, it stimulates digestion and elimination (relaxes gut muscles and colon). One hundred colicky babies that were massaged twice a day, mornings and evenings for one week cried less and experienced less severe symptoms (58).
In conclusion, baby massage is a gentle, safe coping tool for parents less aggressive than pharmacological/medicinal methods. It can easily be incorporated into the baby’s routine. Not all babies and parents will experience the above benefits (root causes may need to be addressed too) but it is certaintly worth a try.
Over the counter (OTC) solutions
Parents commonly resort to OTC medicines and commercial solutions in desperation hoping ‘it will work’. Among the most commonly used are:
- Lactase enzyme. There is some positive evidence that the lactase enzyme helps with colic (60). However, it may have no impact on colic caused by reasons other than a baby’s trouble with lactose (61). In addition, it can be impractical to administer as they enzyme needs to be offered before initiating a feed (at every feed) for best results.
- In bottle-fed babies, there is little evidence a customised bottle design/teat for colic relief (62).
- Colic/reflux pillows or cushions (evidence could not be found)
In conclusion, evidence of the effectiveness of OTC solutions for colic relief is scarce.
Final thoughts

Crying or fussiness in a baby is just like the tip of an iceberg, a strong message that several foundational aspects may be out of balance. Evidently, the reasons for colic are diverse and manifested in a way that is personal to every baby. Listening to the baby, understanding the root causes can help find the right cures.
Based on current evidence and practice, babies should not be let to cry ‘until they grow out of it’. Parents can seek immediate relief through a number of natural, safe options. A combination of root cause and soothing approaches tend to work best.
References
1. https://doi.org/10.1038/s41575-018-0008-7
2. https://doi.org/10.5056/jnm21181
3. https://doi.org/10.3390/ijerph17197011
4. https://doi.org/10.1111/jpc.16174
5. https://doi.org/10.1097/MPG.0000000000000949
6. https://doi.org/10.3390/nu14050974
7. https://doi.org/10.1111/jpc.16174
8. https://doi.org/10.5223/pghn.2017.20.1.1
9. https://doi.org/10.3389/fped.2021.779997
10. https://www.nice.org.uk/cks-uk-only#!scenario
11. https://doi.org/10.1097/MPG.0000000000001075
12. https://doi.org/10.1016/j.jpeds.2017.02.020
13. https://www.nhs.uk/conditions/colic
14. https://doi.org/10.1038/s41575-018-0008-7
15. https://doi.org/10.1097/MPG.0000000000001075
16. https://www.nhs.uk/conditions/colic
17. https://doi.org/10.1007/s00431-017-3026-5
18. https://doi.org/10.1038/ncomms8320
19. https://doi.org/10.1017/S2040174420000227
20. https://doi.org/10.5056/jnm21181
21. https://doi.org/10.1136/bmjopen-2019-035405
22. https://doi.org/10.5223/pghn.2019.22.3.207
23. https://doi.org/10.1097/MPG.0000000000003897
24. https://doi.org/10.3390/microorganisms9122415
25. https://doi.org/10.5223/pghn.2017.20.1.1
26. https://doi.org/10.1097/MPG.0000000000001760
27. https://doi.org/10.3389/fnins.2021.721605
28. https://doi.org/10.1002/icd.688
29. https://doi.org/10.1038/s41390-020-0804-y
31. https://doi.org/10.1038/s41598-017-11509-1
32. https://doi.org/10.3389/fped.2017.00178
33. https://doi.org/10.3389/fnins.2021.721605
34. https://doi.org/10.1002/icd.688
35. https://doi.org/10.3390/healthcare11182600
36. https://doi.org/10.1136/bmjopen-2019-035405
37. https://doi.org/10.1016/j.ctim.2022.102885
38. https://doi.org/10.1002/14651858.CD012459.pub2
39. https://doi.org/10.1177/0890334420959283
40. https://doi.org/10.1016/s0002-8223(96)00013-2
41. https://doi.org/10.1016/s0091-6749(95)70224-5
42. https://doi.org/10.1542/peds.2005-0147
43. https://doi.org/10.1111/apt.15007
44. https://doi.org/10.1038/s41598-020-79022-6
45. https://doi.org/10.3390/nu12092539
46. https://doi.org/10.3390/nu11122964
47. https://doi.org/10.3345/cep.2020.01676
48. https://doi.org/10.3390/microorganisms9122415
49. https://doi.org/10.1542/peds.2017-1811
50. https://doi.org/10.3390/microorganisms10020430
51. https://doi.org/10.1016/j.pedn.2022.12.002
52. https://pubmed.ncbi.nlm.nih.gov/12868253/
53. https://doi.org/10.1155/2021/4889719
54. https://doi.org/10.1155/2021/4889719
55. https://doi.org/10.1097/MPG.0000000000002841
56. https://doi.org/10.1002/14651858.CD012459.pub2
57. https://doi.org/10.3390/ijerph19116378
58. https://pubmed.ncbi.nlm.nih.gov/27453882/
59. https://doi.org/10.1097/MPG.0000000000002841
60. https://pubmed.ncbi.nlm.nih.gov/30504935/
61. https://doi.org/10.1002/jpn3.12144
62. https://doi.org/10.1186/1756-0500-5-150
more Resources
- Free Baby Colic questionnaire. Online assessment to help parents determine the next steps to resolve their babies’ colicky symptoms
- Baby Colic & Early days programme. A 3-week personalised programme to ease and solve colic.
- Baby Colic Relief Programme. A 6-week online programme with a mix of one-to-one consultation, tutorials, videos and group coaching to help parents resolve colic naturally. Coming soon!